One of the first questions many patients have when they begin their journey into stem cell therapy is, “What are the different types of regenerative cells?”
Finding a direct answer to such a simple question can be challenging. Today, we will cut through all the noise and answer that question.
Understanding Cellular Therapy
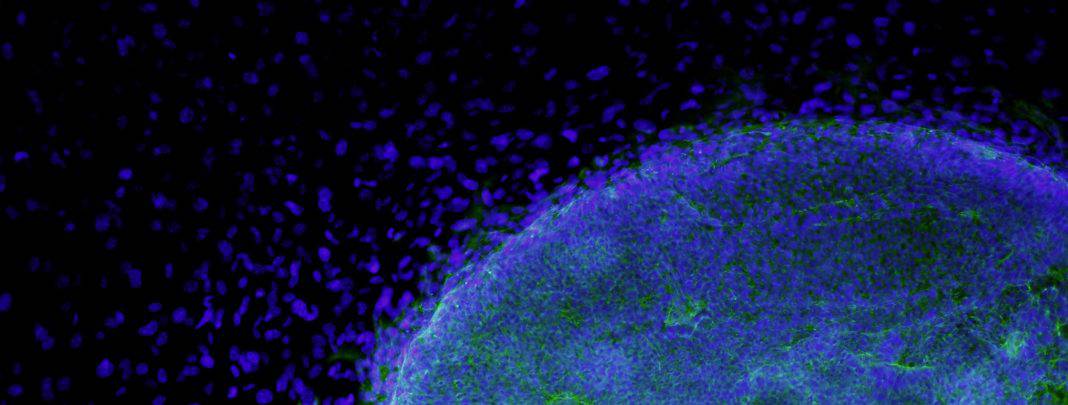
Cellular therapy involves the use of living cells to treat or prevent diseases. These cells can be sourced from a variety of places, including the patient’s own body, donors, or even laboratory cultures. Once administered, these cells can exert therapeutic effects by replacing damaged tissues, modulating the immune response, or delivering therapeutic molecules.
Cellular therapies use cells, rather than chemical compounds or molecules, to fight cancer. Some are made by genetically modifying specific cells from a patient or donor to improve the cells’ cancer-tracking and cancer-attacking ability; others do not involve such modifications.
Not all regenerative cells are created equal.
There is a common misconception that all regenerative cells are created equal. While they all become other types of cells and have the potential to regenerate and renew your cells, they also have some significant differences.
For instance, doctors harvest adipose-derived cells by taking some fatty tissue from your abdomen and obtaining bone marrow stem cells inside your bones. That’s a difference that patients would want to know about up front!
However, both have their uses, and each could be the correct type of stem cell for specific issues, so discuss a customized treatment plan with your doctor. A good regenerative cell therapy clinic will help you understand which types of stem cells are best for your situation, and you’ll reap the benefits of their expert knowledge.
What are the different types of cells used in Regenerative Medicine?
While there are many different types of regenerative cells, we’ll cover those most commonly used in clinical settings.
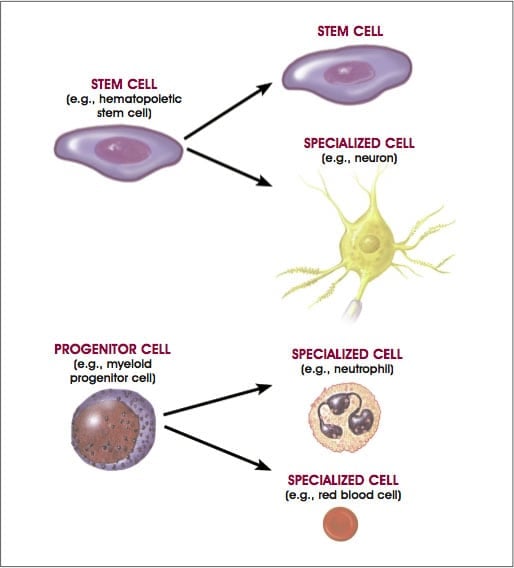
The categories below rely on the differentiation potential of regenerative cells, which refers to their ability to transform into other types of cells.
Multipotent Cells
Multipotent cells can become multiple types of cells within your body.
Until recently, researchers believed that multipotent cells could only become similar types of cells to the type of tissue they were harvested from.
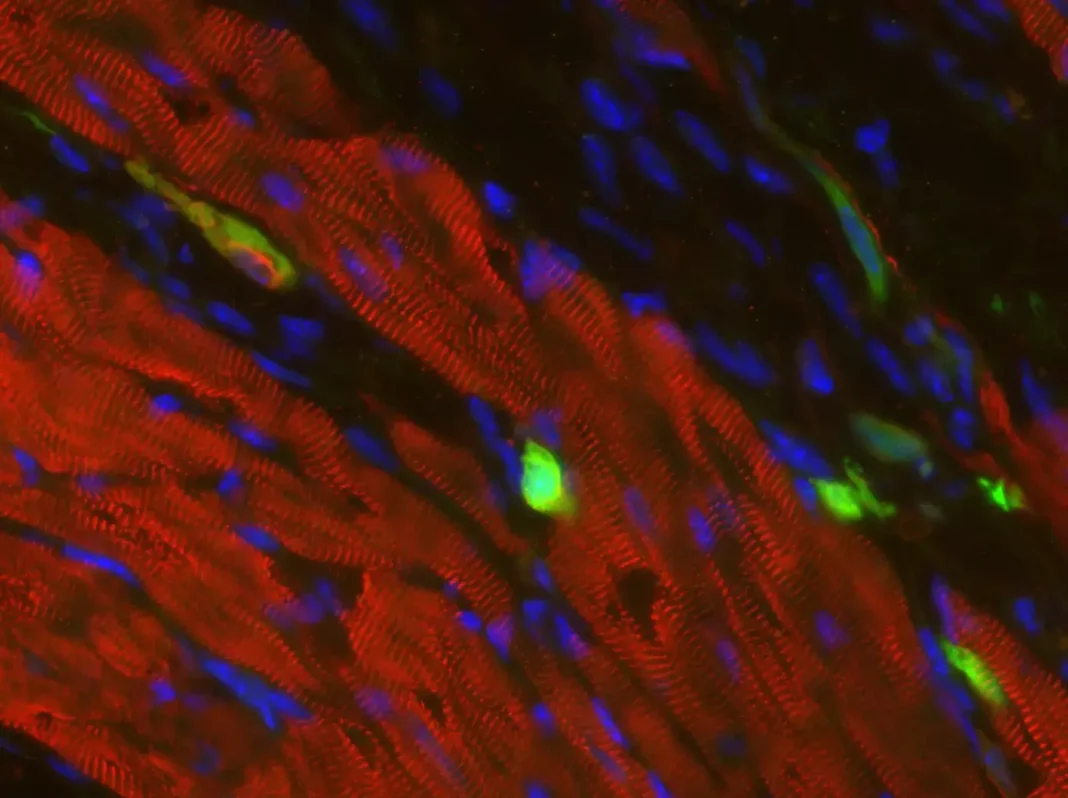
However, in light of recent research, clinical trials are underway to use multipotent cells to repair other tissue types—for instance, regenerating heart and nerve cells.
Adult Cells
Adult cells cause great excitement in the scientific community and are the focus of many regenerative cell research.
While researchers once believed them to be more limited, this new research has revealed more uses for adult cells than was previously believed possible.
Adult cells have more than 60 years of research history, making them one of the best-understood sources for regenerative cell therapy procedures.
- What they are: Undifferentiated, multipotent cells. These cells are still being set on which kind of cell they’ll become, so they can become many different types. For instance, glial cells or neurons.
- Where they’re-they’re from, Juveniles and adults.
- What they’re used for: Replenishing dying cells and regenerating damaged tissue.
- How they work: Capable of infinitely self-dividing, even a few cells from one can grow into an entire organ.
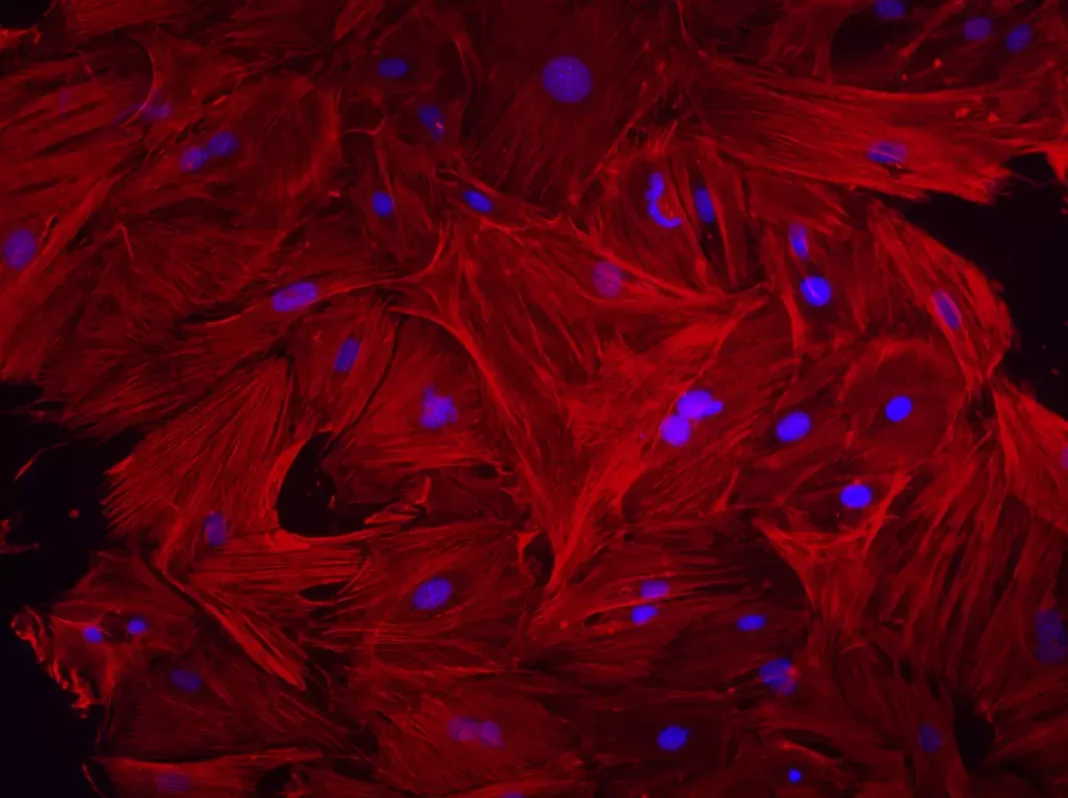
Medicinal Signaling Cells (MSCs)
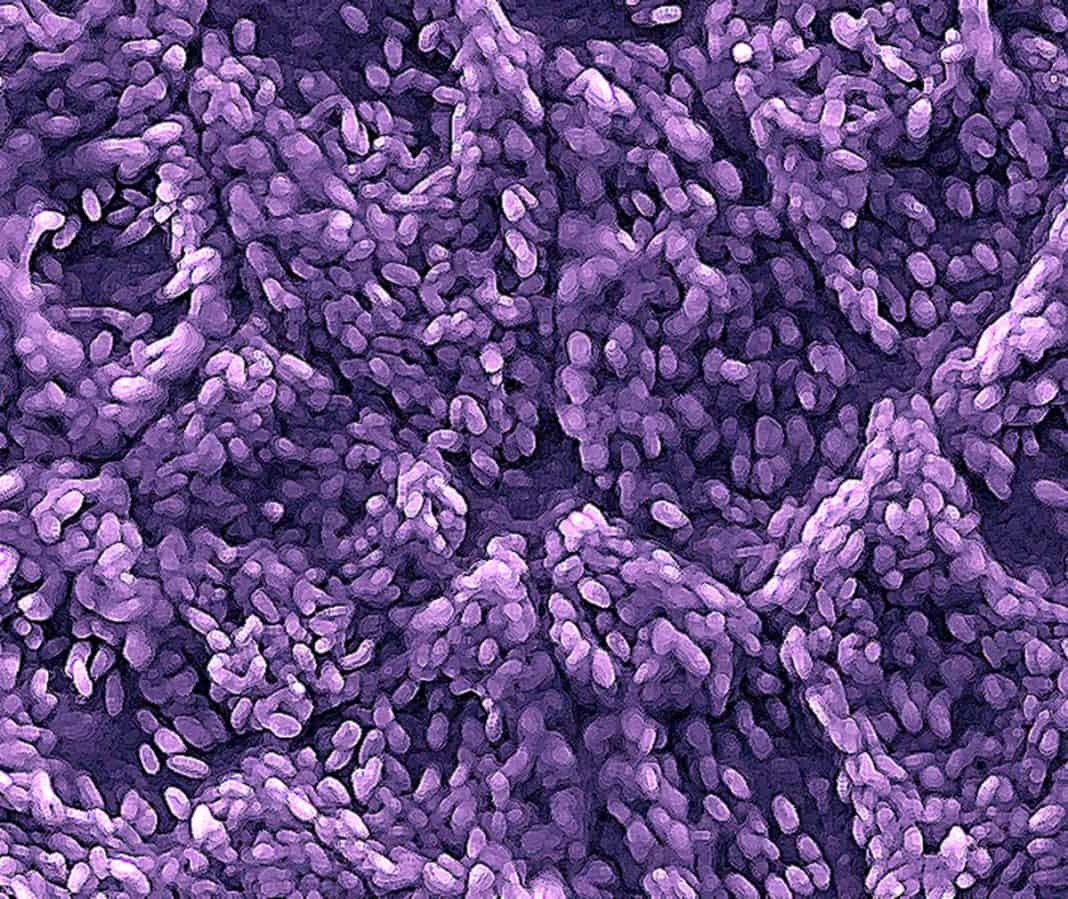
Medicinal signaling cells are a type of cell that comes from various tissues. The unique aspect of medicinal signaling cells is non-blood adult cells that can still form into many different kinds of cells.
These may offer the world the most comprehensive range of ethical uses and have considerable research behind them. In the hands of trained scientists and clinicians, they can be an incredible tool for healing and regeneration.
Since they come from all sorts of tissues and can produce most of the types of cells in the human body, they are an ideal option for adoptive cell therapy. They may treat various diseases, disorders, conditions, and injuries.
- What they are: A type of adult cell, these are multipotent and can become many types of different cells.
- Where they’re-they’re from Adipose (fat) tissue, cord tissue, cord blood, amniotic fluid, skin cells, and bone marrow.
- What they’re used for Potentially treating autoimmune diseases, other conditions and diseases, and musculoskeletal injuries (sports injuries).
- How they work: Like other adult cells, they can self-divide to replicate to higher numbers and, when re-introduced to the body, can become many other types of cells.
Adipose-derived Cells
Since adipose stem cells are a type of mesenchymal stem cell, they carry the associated benefits.
However, due to the ease of acquisition (some fat from the patient’s patient’s abdomen), the procedure allows patients to walk out of the clinic within a few hours.
With no hospital stay or bed rest required, there is minimal interruption to patients’ life. That makes fatty stem cells an especially appealing option to athletes, soldiers, and working people with injuries or conditions affecting their ability to perform their duties.
That said, the benefits have led our clinic to use these cells to treat most patients primarily, but we use other cell types as part of our custom treatment plan whenever it is more beneficial.
- What they are: A mesenchymal cell type, these are more flexible multipotent cells with the capacity for self-renewal. These are the primary type of cells that we use in our clinic.
- Where they’re-they’re from, Amniotic fluid and PRP treatments allow you to walk out of the clinic the same day you come in with the procedure already over. Patients typically return to work on the following day.
- They’re used for various applications, from tissue regeneration in traumatic injuries to many conditions, includingneurodegenerative and endocrine metabolic disorders and post-surgical reconstructions.
- How they work: These medicinal signaling cells can self-divide to replicate to higher numbers. When re-introduced to the body, it can become many other types of cells.
Cord Blood Cells
Cord blood stem cells often treat blood cancers and disorders affecting the hematopoietic (blood-forming) and immune systems.
Since cord blood stem cells can form into blood cells, they may effectively treat leukemias, lymphomas, sickle cell disease, Wiskott-Aldrich syndrome, and more.
We do not use these cells in our clinic for patients needing these specialized treatments that cord blood cells are best suited to. Contact us with any questions.
- What they are: A type of multipotent cell best used for targeted, specialized treatments when necessary.
- Where they’re-they’re from, Cord blood cells are recovered postnatally from the umbilical cord and are a readily available and ethically viable source of cells that could save lives.
- What they’re used for Treating certain conditions and cancers that affect the blood and immune systems, such as leukemias, lymphomas, sickle cell disease, Wiskott-Aldrich syndrome, and more.
- How they work: Since these are medicinal signaling and Hemopoietic cells, they can self-divide to replicate to higher numbers. They contain the blood-forming stem cells that effectively treat blood conditions, even allowing them to treat blood cancers potentially.
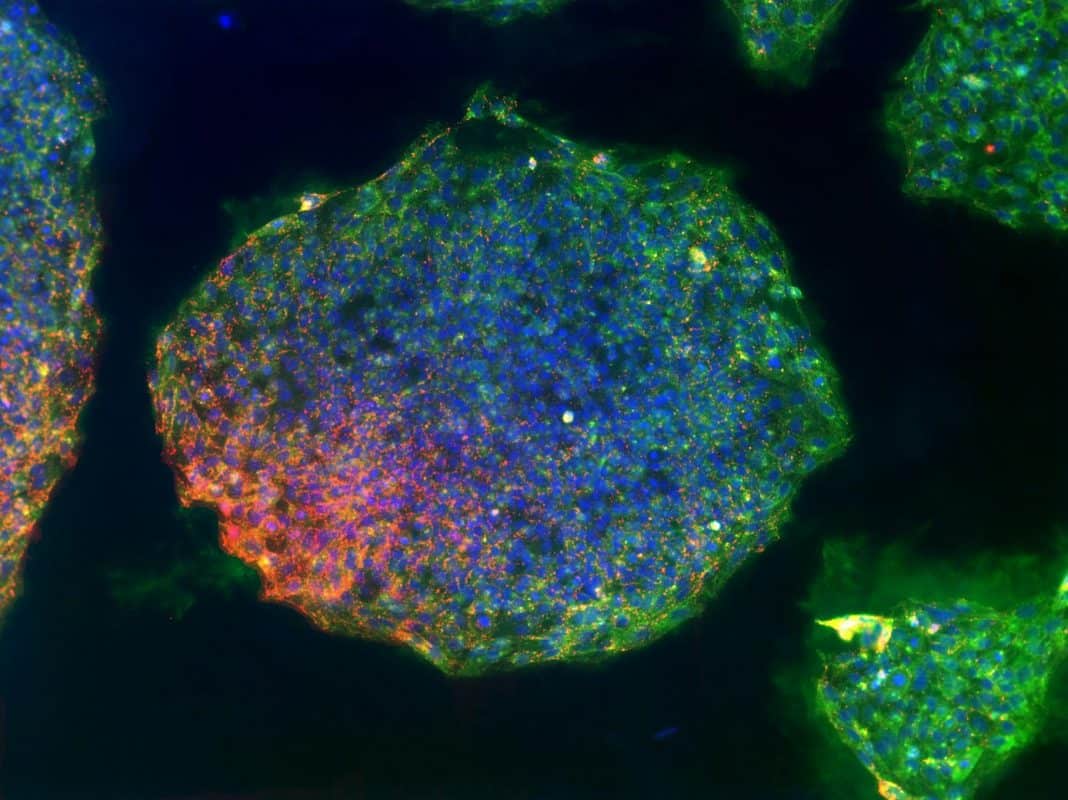
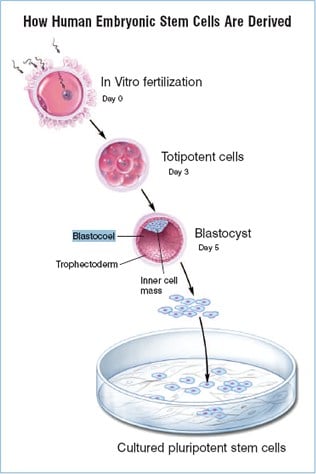
Pluripotent Cells
Pluripotent cells are potent but come with their concerns. These types of cells can become every type of cell that makes up the human body.
Because of this, the medical community closely monitors them. However, they pose complications such as limited availability, ethical controversy, and medical concerns.
Embryonic Cells
Since they are pluripotent and totipotent cells, embryonic sourced cells can become any cell that makes up your body. However, their incredible benefits may also carry potentially dangerous risks.
In addition to ethical concerns, embryonic-sourced cells are believed to risk being rejected by your immune system. More than this, there have been findings ofincreased tumor formation linked to embryonic sourced cells.
Since they carry all these issues and are not your cells, we do not use embryonic stem cells in our clinic.
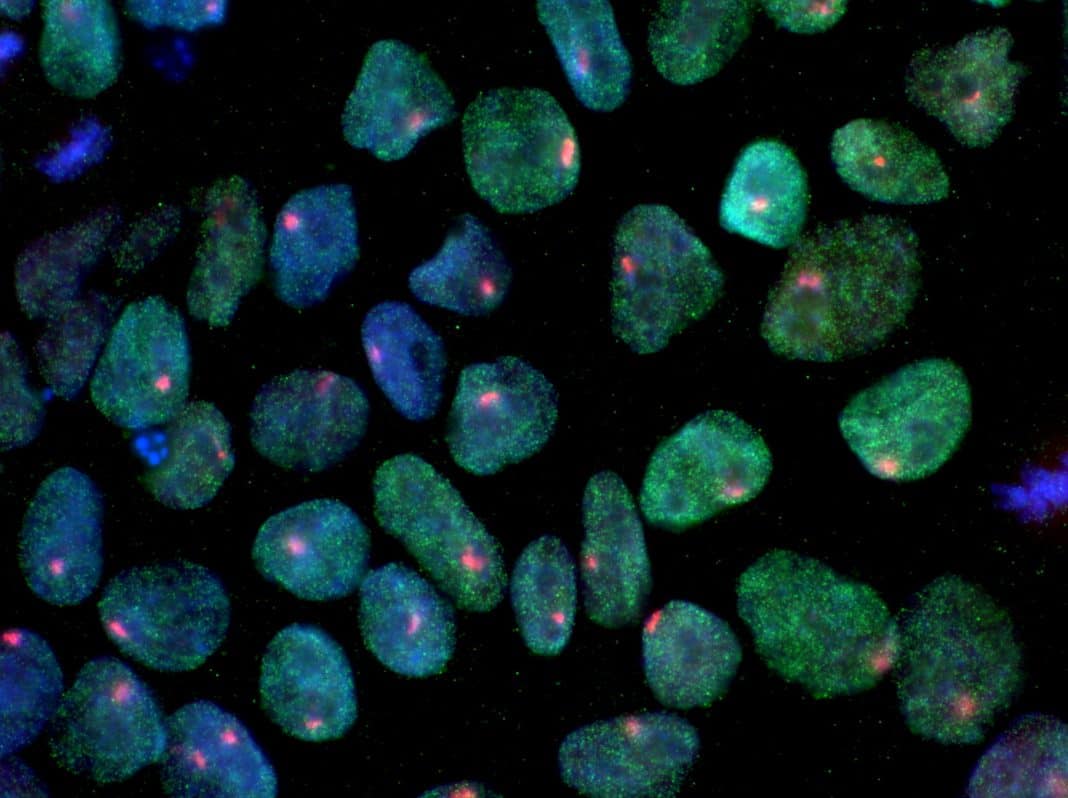
Induced Pluripotent Somatic Cells (iPSCs)
It was 2006 at Kyoto University in Japan, and researchers were on the verge of a breakthrough. Their discovery: introducing specific embryonic genes into a somatic cell can give rise to a new type of cell similar to an embryonic somatic cell.
The publication of this new methodology took the scientific world by storm. These are called induced pluripotent somatic cells because the modified cell can become any cell that makes up the human body.
Because they are in their infancy, there are numerous challenges, and much research is still needed to circumvent their potential risks and increase their efficacy.
Since adult somatic cells have about five decades of additional research behind them and have only recently become widely used in treatments, it may be some time before we see iPSCs reach their full potential.

Different Types of Cellular Therapy
Cellular therapy stands out as a beacon of hope, offering innovative approaches to treating many diseases. From cancer to autoimmune disorders, cellular therapy encompasses a broad spectrum of techniques harnessing the power of cells to heal and regenerate. Let’s delve into the fascinating world of different types of cellular therapy and their potential applications.
1. Stem Cell Therapy
Stem cells are extraordinary entities fundamental to life itself, possessing a unique capability to differentiate into specialized cell types. This remarkable plasticity forms the basis of stem cell therapy, a cutting-edge approach in regenerative medicine. Stem cell therapy harnesses the inherent regenerative potential of these cells to repair and regenerate damaged tissues and organs within the body.
By introducing stem cells into areas of injury or dysfunction, researchers and clinicians aim to stimulate tissue repair processes, enhance healing, and restore normal function. This transformative therapy holds immense promise for treating a wide range of conditions, from degenerative diseases to traumatic injuries, offering hope for improved outcomes and quality of life for patients worldwide.
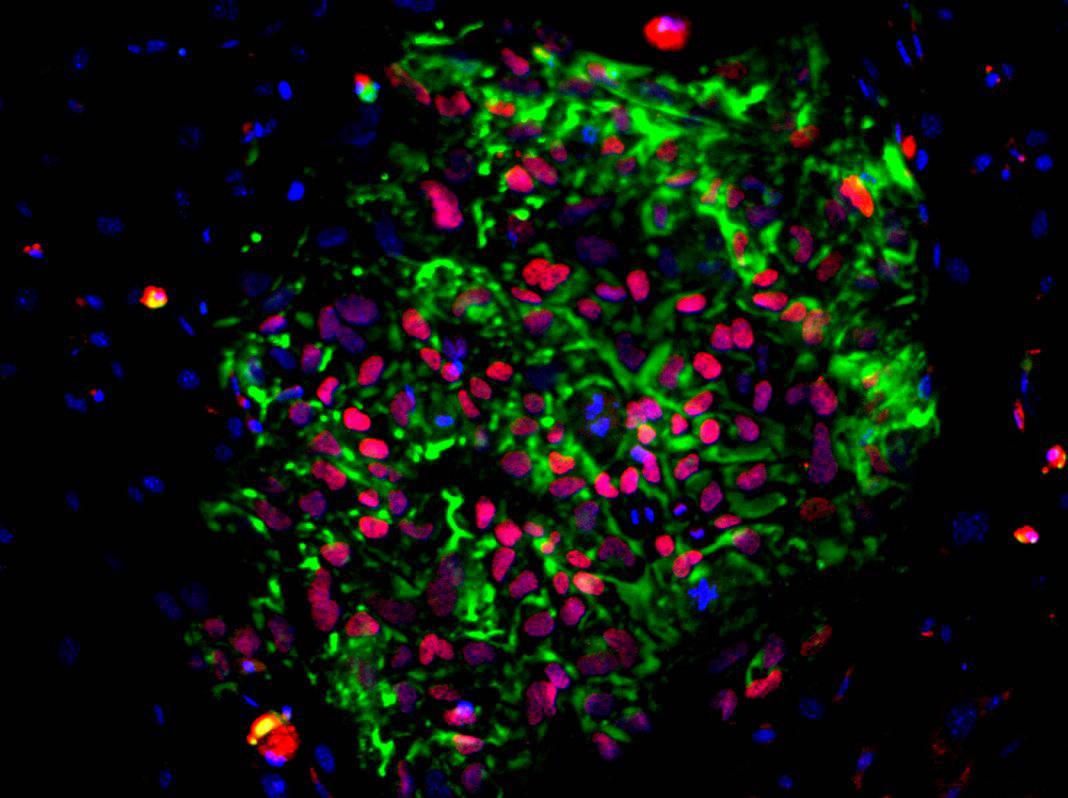
2. CAR-T Cell Therapy
Chimeric antigen receptor T cell therapy has marked a significant milestone in the treatment of some blood cancers, having gained approval as a standard of care. This groundbreaking therapy has spurred the development of a new generation of CAR T-cell therapies, aimed at improving their ability to recognize and combat tumor cells while overcoming the evasive tactics employed by cancers.
Clinical trials of these advanced therapies are now underway, extending their potential application beyond hematological malignancies to include solid tumors like prostate, breast, stomach, and rectal cancers. Concurrently, scientists are dedicated to enhancing the efficacy of CAR T-cell therapies and mitigating their side effects through various avenues.
- Combining CAR T with other therapies – Researchers are investigating strategies to enhance the effectiveness of CAR T-cell therapies by combining them with other immunotherapies, such as checkpoint inhibitors or natural killer (NK) cells. This synergistic approach aims to bolster the immune response against cancer cells and improve treatment outcomes.
- Minimizing side effects – Efforts are underway to mitigate the side effects associated with CAR T-cell therapy. Studies are exploring the use of novel drugs, like defibrotide or anakinra, to manage side effects such as cytokine release syndrome and neurotoxicity. Additionally, researchers are exploring alternate dosing regimens and treatment schedules to optimize the balance between efficacy and safety.
- Timing of CAR T- cell therapy – Research is examining the optimal timing of CAR T-cell therapy administration, investigating whether early-stage intervention or later-stage treatment yields the most favorable outcomes. By elucidating the ideal treatment window, clinicians can maximize the therapeutic benefits of CAR T-cell therapy for patients with various types of cancer.
- Allogeneic CAR T – Trials are exploring the use of allogeneic CAR T cells, which are derived from donor sources rather than the patient’s own cells. This approach offers the potential for off-the-shelf treatments that can be readily available, thereby streamlining the treatment process and improving accessibility for patients in need.
- Correlative research – Scientists are conducting correlative studies to gain insights into how CAR T cells navigate to tumor tissues and exert their anti-cancer effects. By elucidating the mechanisms underlying CAR T-cell therapy, researchers can refine treatment strategies and enhance therapeutic outcomes.
In summary, the ongoing exploration of CAR T-cell therapy holds immense promise for revolutionizing cancer treatment. Through collaborative research efforts and innovative approaches, scientists are striving to optimize the efficacy, safety, and accessibility of CAR T-cell therapies, ultimately improving outcomes for patients with a wide range of malignancies.
3. Tissue Engineering
Tissue engineering represents a groundbreaking interdisciplinary field that merges biology and engineering principles to address the critical need for organ and tissue transplantation. This innovative approach involves the meticulous process of cultivating living cells on specialized scaffolds, which serve as templates for tissue growth. By carefully selecting the cell type and scaffold material and providing the necessary growth factors and biochemical cues, tissue engineers orchestrate the formation of functional tissues and organs in laboratory settings.
This transformative technology holds the potential to revolutionize transplantation medicine by offering tailored solutions for patients suffering from organ failure or tissue damage. Instead of relying solely on donor organs, tissue engineering opens avenues for creating personalized, patient-specific tissues and organs, thereby mitigating the challenges of organ shortage, rejection, and long-term immunosuppression.
With advancements in biomaterials, cell biology, and bioengineering techniques, tissue engineering continues to push the boundaries of what is possible, paving the way for developing novel therapies and regenerative strategies to improve patient outcomes and quality of life.
4. Gene Therapy
Gene therapy represents a revolutionary approach in medicine, offering immense potential for treating a wide range of genetic disorders. By delivering therapeutic genes directly into target cells, gene therapy addresses the root cause of diseases, rather than merely managing symptoms. This innovative strategy opens doors to treating conditions that were once considered untreatable or incurable, providing hope for patients and their families.
Moreover, gene therapy paves the way for personalized medicine, where treatments can be tailored to individual genetic profiles, maximizing efficacy and minimizing side effects. As research and technology in gene therapy continue to advance, the prospects for alleviating genetic diseases and improving patient outcomes are increasingly promising.
5. Immune Cell Therapy
Immune cell therapy is a pioneering approach in modern medicine, leveraging the body’s immune defenses to combat diseases like cancer. Techniques such as adoptive cell therapy involve isolating and cultivating immune cells outside the body, allowing for their expansion and enhancement. Once fortified, these cells are reintroduced into the patient, where they can precisely target and eliminate tumor cells.
This strategy harnesses the innate power of the immune system, offering hope for patients who may not respond to traditional treatments. As research advances, immune cell therapies hold great potential for transforming cancer treatment and beyond, emphasizing the importance of utilizing the body’s own defenses to combat disease.
6. Mesenchymal Cell Therapy
Mesenchymal stem cells, derived from diverse sources such as bone marrow and adipose tissue, demonstrate remarkable regenerative abilities, positioning mesenchymal cell therapy as a promising solution for a broad spectrum of medical conditions. From orthopedic injuries to autoimmune disorders, these cells exhibit inherent anti-inflammatory and immunomodulatory characteristics, enabling them to facilitate tissue repair and regeneration and modulate immune responses.
Such attributes make mesenchymal stem cells valuable candidates for therapeutic interventions, offering potential relief for patients grappling with debilitating conditions by mitigating inflammation and immune dysregulation. As research in this field advances, the utilization of mesenchymal cell therapy expands, opening new avenues for innovative treatments across various medical domains.
7. Dendritic Cell Therapy
Dendritic cells play a crucial role in directing immune responses against pathogens and cancer cells. Dendritic cell therapy is a personalized immunotherapeutic approach where these antigen-presenting cells are loaded with tumor-specific antigens, activating the immune system to target cancer cells effectively. This strategy holds significant promise in cancer treatment by utilizing the body’s own immune defenses.
By precisely stimulating dendritic cells with tumor antigens, this therapy not only initiates an immune response but also enhances its specificity, potentially leading to more effective outcomes. As research in immunotherapies progresses, dendritic cell therapy emerges as a promising avenue for personalized cancer treatment, underscoring the importance of leveraging the immune system’s capabilities in combating cancer.
8. Engineered T Cell Receptor (TCR) Therapy
Engineered T cell receptor (TCR) therapy involves genetically engineering T cells to develop a novel receptor that allows them to bind to specific target proteins on tumor cells. This allows TCR T cells to preferentially target cancer cells while avoiding normal cells, sparing patients from some of the negative effects associated with CAR T-cell therapy.
Furthermore, unlike CAR T cells, which target antigen proteins on the tumor cell surface, TCR treatment targets antigens within the tumor cell, which are only active when the cell is malignant. This, too, may lessen negative effects. Engineered TCR treatment is currently being tested in clinical studies for melanoma, sarcoma, and head and neck cancer.
9. Tumor Infiltrating Lymphocyte (T-IL) Therapy
TIL therapy represents a promising approach in cancer treatment. The process begins by collecting a sample of tumor tissue from the patient, from which T cells are extracted. These T cells undergo multiplication in a laboratory setting, where they are carefully cultured and expanded. Following this, the enhanced TILs are reintroduced into the patient’s body. This therapy has demonstrated notable effectiveness, particularly in the context of melanoma treatment, showcasing encouraging results for some patients. Currently, ongoing clinical trials are exploring the application of TIL therapy in various solid tumors, including cervical and lung cancer. The approach signifies a significant stride in personalized medicine, leveraging the patient’s own immune system to target and combat cancer, offering hope for improved outcomes in the realm of oncology.
10. Natural Killer (NK) Cell Therapy
Natural killer cells play a crucial role in the innate immune system, demonstrating the remarkable capacity to detect and eliminate infected or cancerous cells without prior sensitization. NK cell therapy emerges as an innovative approach to fortifying the body’s inherent defenses against tumors. Whether by enhancing the anti-tumor activity of NK cells through ex vivo activation in the laboratory or direct administration of NK cell-based therapies, this method aims to leverage the innate strength of the immune system in combating cancer.
Through the amplification of NK cell potency, NK cell therapy holds potential for improving the body’s ability to recognize and eliminate cancer cells, presenting a promising avenue for more effective cancer treatment. As immunotherapies advance, NK cell therapy remains a focal point in cancer research, showcasing the prospect of utilizing innate immune responses for therapeutic purposes.
In conclusion, the field of cellular therapy is a dynamic landscape of innovation and discovery, offering hope for patients facing diverse medical challenges. As research and technology continue to advance, the potential applications of cellular therapy are limitless, heralding a new era of personalized and regenerative medicine.
Which types of cells are the best for cell therapy?
The answer to that question will be unique for every individual because there is a different best fit for every situation.
If you’re wondering which types of cellular therapy would be best for your treatment, contact us for a free consultation, and we’ll help you make the right choice.
FAQs
Here are some frequently asked questions about the different types of cellular therapy:
Q. What is CAR-T cell therapy?
CAR-T cell therapy is a combination of immunotherapy and gene therapy used in cancer treatment. It uses the patient’s T cells and genetically modifies them to express chimeric antigen receptors (CARs), allowing for precision targeting of tumor cells. This treatment entails withdrawing T-cells, altering them ex vivo, and returning them into the patient’s body. Its advantage stems from its capacity to specifically target and kill malignant cells. CAR-T treatment has shown effective in treating blood malignancies such as leukemia and lymphoma. Its application has received FDA approval for certain indications, a significant step forward in the development of cell therapies for cancer treatment.
T cells from a patient’s blood are re-engineered to have chimeric antigen receptors (CARs) on their surface. When CAR T cells are re-injected into a patient, the receptors may help the T cells recognize and destroy cancer cells throughout the body.
Q. Can cellular therapy be used to treat cancer?
Yes, cellular therapy can be used to treat cancer. This approach involves using a patient’s own immune cells or genetically modified cells to target and destroy cancer cells. One common form of cellular therapy is CAR-T cell therapy, where T cells are engineered to express chimeric antigen receptors (CARs) that recognize specific proteins on cancer cells, leading to their destruction. This innovative treatment has shown promising results in various types of cancer and continues to be explored in clinical trials for its effectiveness.
Q. How effective is cellular therapy in treating autoimmune diseases?
Cellular therapy has shown promise in treating autoimmune diseases by modulating the immune system’s response. Techniques such as stem cell transplantation, T-cell therapy, and regulatory car t cells aim to restore immune balance and reduce inflammation associated with autoimmune conditions. While effectiveness varies depending on the specific disease and individual patient factors, cellular therapies have demonstrated encouraging results in conditions like multiple sclerosis, rheumatoid arthritis, and lupus. Ongoing research and clinical trials continue to explore cellular therapy’s potential in effectively managing autoimmune diseases.
Q. What are the limitations of current cellular therapy approaches?
Current cellular therapy approaches face limitations such as potential side effects like cytokine therapy release syndrome and neurotoxicity, which can occur with certain treatments like CAR-T cell therapy. Additionally, there are challenges related to the high cost of treatment, limited availability of specialized medical centers offering these therapies, and the complexity of manufacturing personalized cellular products. Furthermore, not all patients respond to these therapies, and there can be variability in effectiveness depending on factors like tumor heterogeneity and immune system function. Research efforts are ongoing to address these limitations and improve the safety, accessibility, and efficacy of cellular therapies for a wider range of diseases.
Q. Are there ongoing research and developments in the field of cellular therapy?
Yes, ongoing research and developments in the field of cellular therapy are robust. Scientists are continually exploring new techniques, such as immunotherapy, gene therapy, and stem cell therapy, to treat various diseases, including cancer, autoimmune disorders, and genetic conditions. Advancements in technology and understanding of cellular mechanisms have led to innovative approaches like CAR-T cell therapy and dendritic cell therapy. These efforts aim to improve treatment efficacy, reduce side effects, and broaden the applicability of cellular therapies for a wider range of patients.
Q. Who are the leading experts in the field of cellular therapy?
In the field of cellular therapy, several leading experts have made significant contributions to research, clinical practice, and innovation. Among them are Dr. Carl June, known for his pioneering work in CAR-T cell therapy for cancer treatment, and Dr. Shinya Yamanaka, whose groundbreaking discoveries in induced pluripotent stem cells (iPSCs) have revolutionized regenerative medicine. Additionally, Dr. Catherine Bollard has made substantial contributions to the development of novel immunotherapies, particularly in the field of pediatric cancers and viral infections. These experts, along with many others in academia, research institutions, and biotechnology companies, continue to drive advancements in cellular therapy, shaping the future of medicine and improving patient outcomes.
Q. Who should consider cellular therapy as a treatment option?
Cellular therapy may be considered as a treatment option for individuals facing various health challenges, including those with chronic conditions, autoimmune disorders, degenerative diseases, or certain types of cancer. Additionally, individuals seeking alternatives to traditional treatments or looking for personalized, targeted therapies may also benefit from exploring cellular therapy options. Consulting with a healthcare provider specializing in regenerative medicine can help determine if cellular therapy is a suitable treatment option based on individual medical history, condition severity, and treatment goals.
Q. Who specializes in administering different types of cellular therapy?
Various medical professionals specialize in administering different types of cellular therapy. For instance, hematologists often oversee stem cell therapies, including bone marrow transplants. Immunologists and oncologists specialize in CAR-T cell therapy, a type of immunotherapy for cancer. Orthopedic surgeons or sports medicine physicians may administer platelet-rich plasma (PRP) therapy for musculoskeletal injuries. Additionally, regenerative medicine specialists or rheumatologists may handle mesenchymal stem cell therapy for conditions like arthritis. The specific expertise required depends on the type of cellular therapy and the underlying medical condition being treated.
Q. Who can provide more information about the risks and benefits of cellular therapy?
Medical professionals, particularly specialists in fields like oncology, regenerative medicine, and immunology, are best equipped to offer comprehensive information about the risks and benefits of cellular therapy. These professionals have in-depth knowledge of the latest research, clinical trials, and treatment protocols related to cellular therapy. They can assess individual patient cases, discuss potential risks and benefits, and provide personalized guidance based on each patient’s unique medical history and condition. Additionally, reputable healthcare institutions and research organizations may offer educational resources and support to help patients make informed decisions about cellular therapy.
Q. What is an example of cellular-based therapy?
An example of cell-based therapy is stem cell therapy. This approach involves using stem cells, which have the unique ability to develop into different types of cells in the body, for regenerative purposes. In stem cell therapy, these cells are harvested from various sources such as bone marrow, adipose tissue, or umbilical cord blood, and then administered to patients to repair or replace damaged tissues and organs. Stem cell therapy shows promise in treating a wide range of conditions, including heart disease, spinal cord injury, and certain types of cancer.
Q. What are examples of cellular immunotherapy?
Examples of cellular immunotherapy include CAR-T cell therapy, where a patient’s T cells are engineered to target and destroy cancer cells, and dendritic cell therapy, which involves stimulating a patient’s dendritic cells to enhance the immune response against cancer or infectious diseases. These approaches harness the power of the immune system to combat diseases and have shown promising results in treating various cancers and other conditions.
Consult with Dynamic Stem Cell Therapy today!
Experience the transformative potential of stem cell therapy with Dynamic Stem Cell Therapy. Our dedicated team specializes in harnessing the regenerative power of stem cells to address a wide range of conditions, from orthopedic injuries to degenerative diseases. Whether you’re seeking relief from joint pain, exploring alternatives to traditional treatments, or looking to optimize your body’s natural healing processes, our tailored therapies offer personalized solutions to meet your unique needs.
At Dynamic Stem Cell Therapy, our mission is to provide cutting-edge care that empowers individuals to live their best lives. With a focus on regenerative medicine, we offer a variety of stem cell therapies tailored to address a wide range of conditions, from orthopedic injuries to degenerative diseases like cartilage degradation. Our expert care team, led by experienced MDs, is dedicated to staying at the forefront of research and innovation, ensuring that our patients have access to the latest treatment options.
From our state-of-the-art lab to our comprehensive testing program, we are committed to delivering personalized care that meets the unique needs of each individual. Whether you’re exploring stem cell therapy as an alternative to traditional treatments or seeking relief from chronic pain, our team is here to provide the information and support you need to make informed decisions about your health. Contact us today to learn more about our programs and schedule a consultation with our compassionate care team.